Wisdom Tooth Removal - North Shore Oral and Maxillofacial Surgery
Home » Procedures »
Wisdom teeth (also called third molars) usually do not push through the gums until people in their late teens, twenties or even later. They are usually the last teeth to erupt.
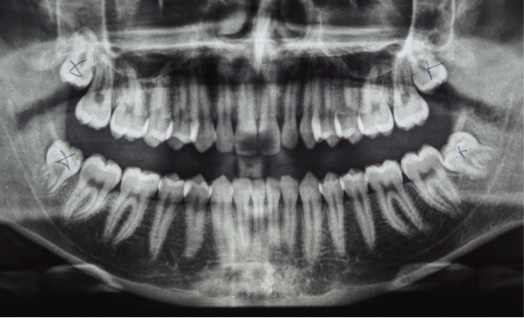
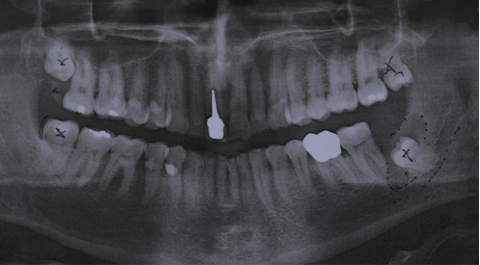
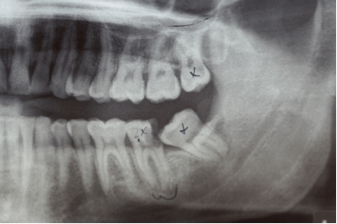
Most people have four wisdom teeth. There are however many variations from no wisdom teeth at all to having more than one tooth in an area, so that patients may have five, six or more wisdom teeth. Often there is little space left behind the second molars for the wisdom teeth to come through. In that case the wisdom teeth may be wedged in or “impacted”.
Impacted wisdom teeth may cause symptoms with pain and infection. That is usually the time to assess the wisdom teeth and the need for their removal. Once impacted wisdom teeth are diagnosed, your dentist usually will refer you to an oral and maxillofacial surgeon for removal of the wisdom teeth. Usually the whole jaw is assessed regarding impacted wisdom teeth and need for their removal. Some times there may be deeply impacted wisdom teeth with a good chance of never causing symptoms, so that they may not have to be removed. Others may be in a position that there is a high risk for later complications, so that there may be the recommendation for removal of all wisdom teeth, even if only one of them has caused symptoms.
Usually a full mouth panoramic x-ray (OPG) is taken, to assess the wisdom teeth and the need for their removal. This shows all teeth and possible cysts, that can be associated with unerupted teeth. This would be another reason for removal of a wisdom tooth, as a related cyst can grow and replace the existing bone (bone resorption). This can lead to risk of fracture, if a lot of bone is resorbed.
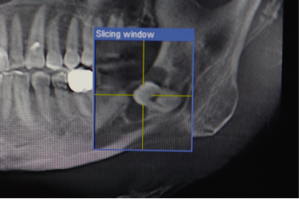
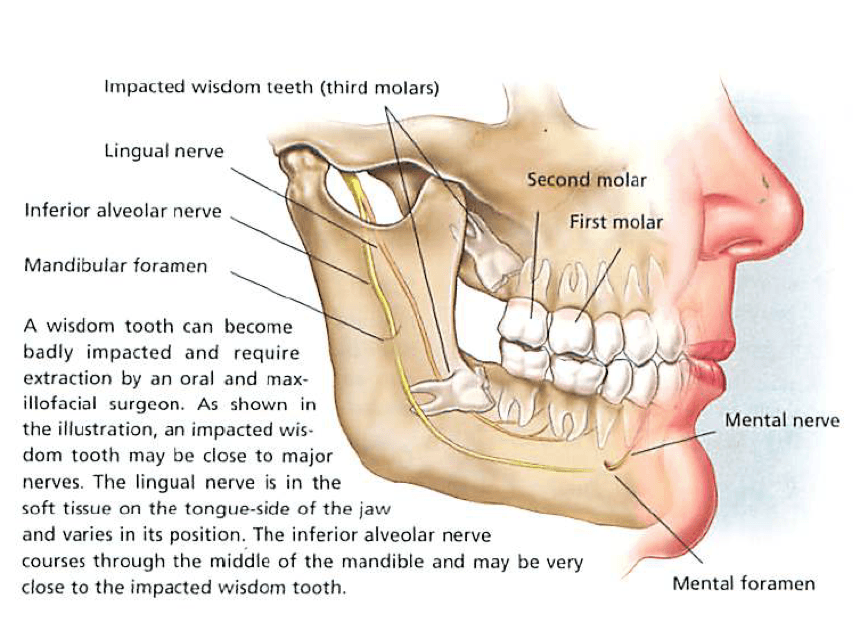
If there is a close relation to the inferior alveolar nerve, further diagnostic with a cone beam scan (3 diomensional scan) may be necessary to clearly show the relationship to the nerve and to reduce the risk for any damage.
Other symptoms beside infection can be pressure of the wisdom teeth, causing pain in the jaws or possibly headaches. If wisdom teeth have been persisting for a long time they can cause decay and pain on adjacent teeth.
If a wisdom tooth area is infected, local symptomatic treatment with salty water mouth rinses and antibiotic treatment will help to settle the infection. After the infection is settled, the wisdom teeth can be removed.
Additionally there may be an indication for removal of wisdom teeth even without any symptoms. If there are impacted wisdom teeth after orthodontic treatment, there may be a risk, that the wisdom teeth push the other teeth forward and cause crowding.
After the decision has been made to get wisdom teeth removed,the question is, how this should be done.
It could be done with local anaesthesia with injection to numb the area of the wisdom tooth and surrounding tissues. This can be done for single teeth and if the removal of the tooth is not difficult.
If there are more teeth that have to be removed and the surgery is more difficult, generally a sedation or full anaesthesia is recommended. In this case we allways use a fully equipped day surgery with anaesthesist, who exclusively looks after your anaesthesia, while the teeth are removed. Afterwards you wake up, and the surgery is done. That is the most convenient and most safe way of removal of your wisdom teeth, using a day surgery with all clinical monitoring and dedicated anaesthesist for you. After completed surgery you then have to stay for an hour or so in the recovery, before you can be discharged home. Due to the anaesthesia you allways will need a carer to come with you.
After the operation there always we be some numbness of lips, gums and teeth due to the local anaesthesia. This will last for some hours depending on type and amount of the local anaesthetic. During this time you should be careful not to bite your lip or tongue. For further details look at the postoperative instructions shown elswhere on this website..
Possible complications for removal of wisdom teeth are due to the neighbouring structures.
For the lower wisdom teeth is the inferior alveolar nerve running along in some association to the roots. If there is need, additional scans are performed to clearly show the nerve poisition and reduce any risk for nerve damage as much as possible. Some times with close association there may be some bruising of the nerve, leading to numbness or tingling of the lower lip, gums and teeth suplied by this nerve. This usually revovers within days to weeks. Only rarely it will take longer. The revcovery can be accompanied by tingling or uncomfortable sensations, before the normal feeling returns. In very rear cases this can take longer or be permanent with some defect ion sensitivity.
The second nerve to mention is the lingual nerve passing by on the lingual side of the jaw, sometimes very close to the wisdom tooth. Again the removal of the wisdom tooth can cause some bruising, leading to numbness of the tongue and possible impairment of taste. These symptoms are even less frequent than for the inferior alveolar nerve and are temporary only in the most cases as well.